Key Takeaways
- IBS is a chronic digestive disorder causing colon pain, bloating, constipation or diarrhea, and painful bowel movements.
- It results from multiple factors, including gut-brain axis dysfunction, gut microbiota imbalance, irregular intestinal muscle activity, and stress.
- IBS symptoms in females can be influenced by hormonal and psychological factors, requiring personalized management.
- Recognizing early signs of gastrointestinal disease and avoiding IBS trigger foods can improve IBS relief and reduce IBS flare ups, with timely care available at our Amarillo emergency room.
What causes IBS?
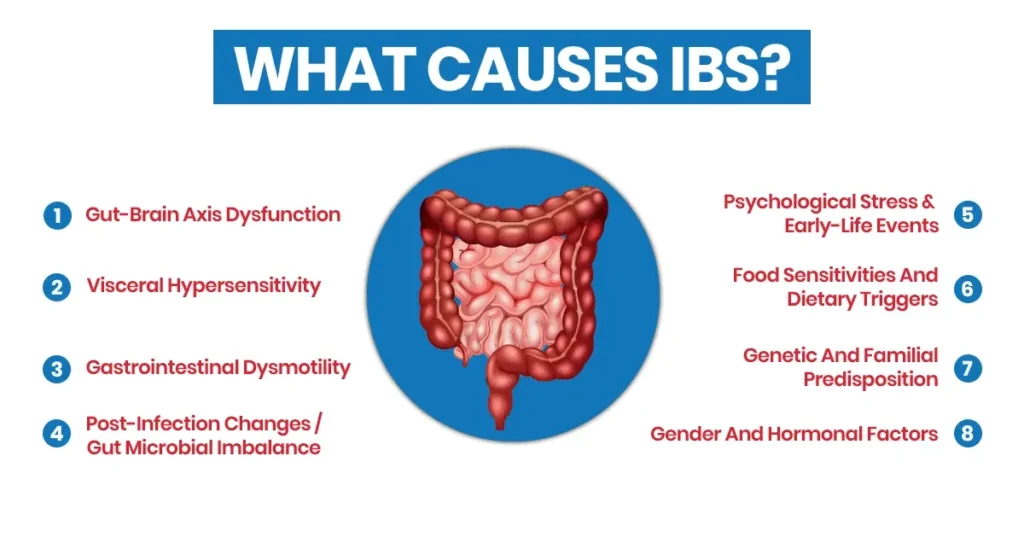
Irritable Bowel Syndrome (IBS) arises from a combination of factors, including gut-brain axis dysfunction, altered intestinal motility, and changes in gut microbiota. A study published on PubMed found that approximately 33% of participants experienced IBS symptoms, highlighting the role of gastrointestinal sensitivity and environmental triggers in its development. This research emphasizes that IBS is a multifactorial disorder influenced by both physiological and lifestyle factors.
IBS symptoms
- Abdominal pain or colon pain.
- Bloating and a sensation of bloated gut pain.
- Alternating constipation and diarrhea or constipation after diarrhea.
- Painful bowel movements.
- Gas, cramping, or discomfort.
- Urgency or incomplete bowel movements.
- IBS flare-up periods with symptom variability.
Gut‑brain axis dysfunction
Disrupted communication between the gut and brain can cause the intestines to react abnormally to normal digestive processes. This may lead to colon pain, bloating, and irregular bowel movements. Emotional stress can directly influence gut-brain signaling, worsening IBS symptoms. Maintaining a regular sleep schedule can support gut-brain balance and reduce symptom severity.
Visceral hypersensitivity
People with IBS often have an oversensitive gut, making normal bowel activity feel painful. This can increase bloating and discomfort. Even minor gas accumulation may trigger significant colon pain in sensitive individuals. Gentle abdominal massage or warm compresses can sometimes ease discomfort in sensitive areas.
Gastrointestinal dysmotility
Irregular intestinal muscle activity can speed up or slow down digestion, causing diarrhea, constipation, or painful bowel movements. Abnormal contractions may occur in response to meals or stress, intensifying symptoms. Eating smaller, more frequent meals can help regulate intestinal motility and reduce flare-ups.
Post‑infection changes / Gut microbial imbalance
A prior gastrointestinal infection can alter gut function long-term, sometimes leading to IBS. Imbalances in gut microbiota may increase intestinal sensitivity and inflammation. Antibiotic use or severe infections can further disrupt microbiome balance, triggering flare-ups. Probiotic-rich foods or supplements may help restore healthy gut bacteria.
Psychological stress & early-life events
Chronic stress or early-life trauma can disrupt gut-brain communication, worsening IBS symptoms. Emotional stress may trigger an IBS flare-up and painful bowel movements. Mind-body techniques like meditation can help modulate stress-induced gut responses. Regular relaxation exercises can improve both mental and digestive health over time.
Food sensitivities and dietary triggers
Certain foods, such as dairy, gluten, or gas-producing items, may worsen IBS symptoms. IBS trigger foods can cause bloating, diarrhea, or constipation. Food intolerances vary individually, making personalized dietary plans essential for relief. Keeping a food diary can help identify patterns and prevent flare-ups.
Genetic and familial predisposition
Having a family history of IBS increases the likelihood of developing the condition. Genetic factors may influence gut sensitivity and motility. Some genetic variations may affect serotonin regulation in the gut, impacting bowel function. Understanding family medical history can help guide early preventive strategies.
Gender and hormonal factors
Hormonal fluctuations in females can affect gut motility and sensitivity, increasing IBS risk. Women are more likely to experience bloating and painful bowel movements. Hormone changes during menstruation or menopause can temporarily worsen IBS symptoms. Tracking symptoms in relation to the menstrual cycle can help in managing IBS more effectively.
When Is Irritable Bowel Syndrome an Emergency?
Although IBS is usually not life-threatening, certain symptoms require urgent attention. Severe or sudden changes in bowel habits, bleeding, or intense pain may indicate a more serious condition. Alarm signs may include:
- Severe, persistent abdominal pain.
- Blood in stool or dark, tarry stools.
- Unintended weight loss.
- Fever alongside digestive symptoms.
- Signs of dehydration (dizziness, fainting).
If you notice any of these signs with your digestive problems, contact the Exceptional Emergency Centers immediately.
How IBS Is Diagnosed
Diagnosis begins with reviewing symptoms, medical history, and a physical exam. This process rules out other conditions and helps identify patterns like bloating, constipation after diarrhea, or painful bowel movements. Diagnostic methods may include:
- Clinical History & Symptom Evaluation: Detailed discussion of abdominal pain, bowel habit changes, IBS symptoms in females, dietary triggers, and stress.
- Use Of Diagnostic Criteria (E.G., Rome Criteria): Standardized tools like Rome IV help confirm IBS based on symptom frequency and duration.
- Exclusion Of Other Conditions: Blood tests, stool tests, and imaging ensure that digestive problems are not caused by infections, inflammation, or structural issues.
- Additional Testing If Needed: Colonoscopy or imaging may be performed if alarm signs or severe symptoms are present.
How Can IBS Be Treated?
Managing IBS often combines lifestyle changes, dietary modifications, medications, and psychological approaches to reduce IBS flare-ups and improve IBS relief.
- Dietary Adjustments & Identifying Ibs Trigger Foods: Avoiding problematic foods such as dairy, gluten, and gas-producing items reduces bloating and painful bowel movements.
- Stress Management & Psychological Support: Mindfulness, counseling, or cognitive behavioral therapy can improve gut-brain communication and reduce flare-ups.
- Medications For Gut Motility & Pain: Antispasmodics, laxatives, antidiarrheals, or low-dose antidepressants can relieve constipation, diarrhea, or abdominal pain.
- Probiotics And Gut Microbiome Support: Supporting a healthy gut microbiota may improve digestion and reduce IBS symptoms.
- Lifestyle Changes: Regular activity, proper hydration, and a balanced fiber intake support gut health and digestive function.
Get Expert IBS Care at Exceptional Emergency Centers
If you experience severe or persistent IBS symptoms, seeking professional emergency care at Exceptional Emergency Centers is essential. Our team provides rapid assessment to manage colon pain, painful bowel movements, and other digestive problems. Early evaluation helps prevent complications and supports better digestive health.
Our specialists can help answer the question, “What causes irritable bowel syndrome?” by identifying triggers such as stress, diet, and hormonal factors. We offer personalized care and guide you on IBS relief strategies. Whether it’s frequent flare-ups or bloated gut pain, we provide professional support for improved digestive function.

